Pituitary adenomas are benign tumors of the pituitary gland.
Treatment can be complex, but the vast majority of cases evolve well.
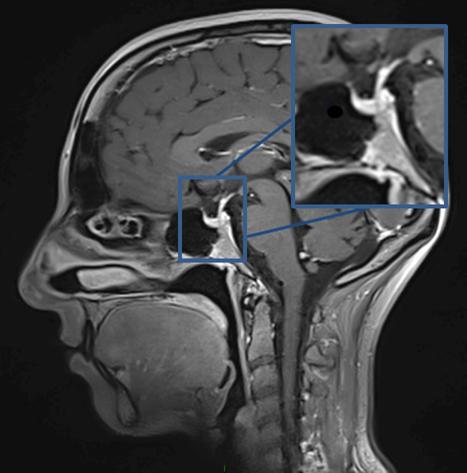
Cerebral MRI, sagittal section: Hypopyse and pituitary stalk.
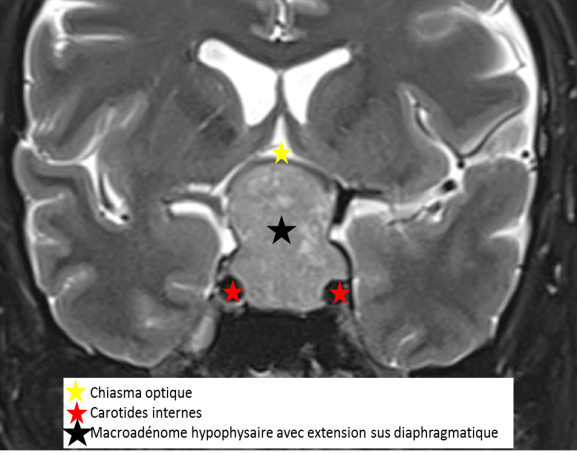
Brain MRI, coronal section: pituitary macroadenoma.
Pituitary adenomas are often discovered incidentally during brain imaging (CT or MRI) performed for another reason.
Pituitary adenomas can cause 3 main types of symptoms depending on their type and size:
Symptoms related to the compression exerted by the tumor on surrounding structures:
– Visual disturbances (linked to compression of the optic chiasma, located a few millimetres above the pituitary gland)
– Reduced visual field
– Decreased visual acuity
– Headaches
– Symptoms associated with compression of the nerves that run along the pituitary into the cavernous sinus and control eye movements. This is most often double vision or drooping of the eyelid. These symptoms are rare in pituitary adenomas, and most often indicate abrupt necrosis and/or bleeding within the tumor.
Symptoms related to excessive secretion of a hormone by the tumor:
– hypersecretion of prolactin or “hyperprolactinemia”, responsible for the disappearance of menstrual periods (secondary amenorrhea), milky secretion from the breasts (galactorrhea) or sexual disorders,
– acromegaly secondary to growth hormone hypersecretion, responsible for progressive and insidious thickening of the face and extremities, hypersudation, carpal tunnel syndrome, joint pain, hypertension and diabetes,
– hypercorticism (Cushing’s syndrome) secondary to hypersecretion of ACTH stimulating adrenal cortisol production, manifesting as android obesity with hypertension, diabetes, fatigue, facial flushing and sometimes psychiatric disorders.
– more rarely, hyperthyroidism secondary to TSH hypersecretion by a thyrotropic adenoma.
Symptoms related to insufficient secretion of certain hormones normally secreted by the pituitary gland:
A reduction or defect in the secretion of hormones normally secreted by the front part of the pituitary gland (hypopituitarism) results, when global, in fatigue, paleness, sexual problems and thin skin. Growth hormone deficiency in children leads to stunted growth. Thyroid hormone deficiency leads to paleness, weight gain, constipation and depression. Gonadotropic insufficiency is linked to a defect in the production of hormones that stimulate sex hormone production by the ovaries and testes. It leads to signs of hypogonadism (absence of puberty, amenorrhea, impotence, infertility); Corticotropic insufficiency, the most life-threatening form, leads to asthenia, arterial hypotension and digestive disorders in the event of decompensation.
In the presence of these symptoms, clinical analysis can point to a pituitary pathology, and in case of suspicion, a biological workup should be performed as a priority. When this suspicion is confirmed, the reference radiological examination is pituitary MRI.
There are several histological subtypes corresponding to different clinical presentations:
Secretory or functional adenomas
– Prolactin adenoma (PRL) is the most common, accounting for 60% of all adenomas (female-to-male ratio: 10:1, mean age at diagnosis: 32).
– Growth hormone (GH)-secreting somatotropic adenomas account for around 13% of all adenomas; age at diagnosis is 47, with a frequent variant, the somatoprolactin adenoma, secreting PRL and GH (50% of somatotropic adenomas).
– Corticotropic adenomas are usually small (<10mm) or “micro-adenomas” and secrete ACTH. It accounts for 6% of all adenomas. Macroadenomas are less common.
– TSH-secreting thyrotropic adenomas are rare (<1% of all adenomas). It is most often accompanied by hyperthyroidism, but can be silent and multi-creative (TSH-GH and TSH-PRL).
Non-secreting or non-functioning adenomas
They account for 30% of pituitary adenomas. The term “non-functional” should be preferred, as in around a third of cases, there is a hormonal expression, without clinical translation, but which can serve as a biological marker. Most of these tumors are gonadotropic adenomas.
Silent adenomas
They are less frequent. These are adenomas presenting as a tumor compression syndrome without any specific clinical picture of hypersecretion, but which are immunocytochemically positive for ACTH, GH or TSH, or even multihormonal (GH and PRL or TSH and GH). Biologically, they either do not secrete a hormone, or more frequently, they secrete an inactive pro-hormone, which explains the absence of clinical signs, or a low-level but measurable hormone (ACTH hypersecretion without hypercorticism is the most frequent example).
Aggressive or atypical adenomas and carcinomas
The frequency of aggressive adenomas is still poorly understood. Only 0.2% of tumors metastasize during the course of their evolution and are considered to be carcinomas: most are secretory – 36% PRL, 30% ACTH – and only 23% are non-secretory. These metastases, which are never inaugural, occur 5 to 16 years after the onset of the clinical history, and involve either the nervous system, with dissemination via the cerebrospinal fluid (CSF), or various organs: lungs, bones, liver or even lymph nodes.
Who’s concerned?
Pituitary adenomas account for between 10 and 20% of adult intracranial tumors. These tumors have an incidence of 4/100,000 inhabitants, with an increasing trend towards incidental findings.
This is a rare tumor (2.7% of supratentorial tumors) in children, whose most common tumor of the pituitary region is the craniopharyngioma.
How is the diagnosis made?
When faced with a set of endocrine, neurological and ophthalmological symptoms, your doctor will order a cerebral MRI scan to confirm the existence of a pituitary lesion, leading to a consultation with a neurosurgeon or endocrinologist.
Endocrine check-up
The endocrine workup will be initiated either because the patient presents with an endocrine syndrome or because a lesion in the pituitary region has been discovered on imaging. As a matter of routine, this check-up includes assays of the main hormonal axes (Prolactin; TSHus; T4l; T3l; FSH; LH; Estradiol/ Testosterone; GH; Igf1; Cortisolemia).
An endocrinology consultation with Dr. LALOI-MICHELIN, our referent, will only be organized preoperatively in cases of secretory pituitary adenomas or in the event of hormonal insufficiencies on the workup. If necessary, hormone replacement or medical treatment of the secreting adenoma may be considered before the operation.
Radiological assessment
Cerebral MRI remains the gold standard for exploring pituitary lesions. This examination must be optimal in order to have a precise anatomical description, making it possible to define the limits of the adenoma with :
- its extension into the sella turcica
- diaphragm up and supra-diaphragmatic extension
- the cavernous sinuses laterally,
- healthy pituitary gland
- opto-chiasmatic pathways,
- the diencephalon.
Cerebral CT with angioscan in bone windows can be requested and used in neuronavigation to guide surgery. This examination provides additional information, particularly on bone involvement in the pituitary gland.
The radiology of the pituitary region is very rich and requires a great deal of experience on the part of the radiologist. To this end, files are reviewed with a neuroradiologist with expertise in this pathology.
Neuroradiological assessment
The neuro-ophthalmological syndrome will be investigated according to the patient’s visual complaints and, above all, the extension of the pituitary adenoma to the opto-chiasmatic pathways and/or to the cavernous sinus on cerebral MRI. The neuro-ophthalmological examination will include a visual acuity measurement, a fundus and a visual field, or even an OCT to assess optic nerve compression, and possibly a Lancaster test if oculomotor nerve damage is suspected.
What treatments are available?
Care may consist of:
- neuroradiological monitoring in the case of non-secreting adenomas;
- medical treatment for functional adenomas when antagonistic medical treatment is possible; in this case, the patient is referred to an endocrinologist.
- excision surgery for progressive adenomas, adenomas resistant to treatment, adenomas with compression of the opto-chiasmatic pathways;
- radiotherapy or radiosurgery for inoperable adenomas, postoperative residues for which surgical revision is impossible or high-risk, and aggressive adenomas.
Surgical treatment
The neurosurgeon is involved in the management of patients with pituitary adenomas, including those requiring only neuroradiological monitoring. Pituitary adenoma is a benign tumor that develops slowly. Neuro-radiological monitoring enables us to estimate the evolutionary curve, so that the indication for surgery can only be made in the event of significant tumor growth, and before the adenoma has spread significantly; the most complete excision possible can then be envisaged, while preserving the physiological endocrine functions of the pituitary gland. In the case of a microadenoma ( < 10 mm), the aim of surgery is to remove the entire tumour and cure it.
-

Pituitary adenoma
Consultation with a neurosurgeon
During this consultation, you will be offered a complementary work-up if necessary, and the relationship between your symptoms and the lesion will be explained, as well as the natural history of these adenomas and their relationship with neighbouring structures (invasive or non-invasive nature of the adenoma). The neurosurgeon may decide to perform endoscopic endonasal surgery. The decision to intervene is usually taken following a multidisciplinary consultation meeting, during which the case is discussed in the presence of neurosurgeons, endocrinologists and neuroradiologists.
Why endoscopic endonasal surgery?
Today, the vast majority of pituitary adenomas are operated on endoscopically via the endonasal route. Unlike the microscope, where the surgeon’s eye remains outside the nose, giving only a very limited view of the back of the nasal cavities, the endoscope takes the surgeon’s eye deep into the nasal cavity, giving a panoramic view of the region and the lesion. Thanks to 30° and 45° endoscopes, it also enables us to see laterally and upwards, and thus better appreciate any tumour extensions. The use of minimally invasive approaches that respect the nasal cavities has significantly reduced the rhinological morbidity of this surgery and increased postoperative comfort for patients.
Preoperative consultation and assessment
- Radiological check-up,
- Consultation with endocrinologist if necessary,
- Neuro-ophthalmological consultation if necessary,
- Anesthesia consultation for surgery.


